Dissociative Seizures: Understanding the Hidden Struggle Behind Misdiagnosis
Seizures are considered one of the most concerning medical problems. A person may become unable to regulate their thinking or movements during a seizure. But not every seizure is what it seems to be. While many people believe seizures are caused by epilepsy, there is another form of seizure that appears quite similar but has an entirely different cause. These are known as dissociation seizures, and epilepsy gets frequently incorrectly diagnosed and misinterpreted as these.
In this blog, we'll dive deep into what dissociative seizures are, how they differ from true epileptic seizures, and why it’s crucial to make the right diagnosis. Misdiagnosis can lead to unnecessary treatments, prolonged suffering, and emotional distress. We will also discuss the connection between dissociative seizures, anxiety, and depression and how these illnesses are addressed together.
What Are Dissociative Seizures?
Seizures that mimic epilepsy but are brought on by psychosocial variables as opposed to aberrant electrical activity in the brain are referred to as dissociative seizures, or psychogenic non-epileptic seizures (PNES). These seizures can include jerky movements, convulsions, and loss of consciousness, similar to epileptic seizures. However, the main distinction is that they are caused by emotional stress, trauma, or psychological conflict.
In India and around the world, many patients are misdiagnosed with epilepsy when they are actually having dissociative seizures. Due to this error in diagnosis, they may be given anti-epileptic medication, which has no effect on treating dissociative seizures and could have unneeded adverse effects.
Real-Life Story: Meera's Journey
Take the example of Meera, a 24-year-old woman from Delhi. She began experiencing seizures at the age of 18. Initially, doctors diagnosed her with epilepsy and prescribed anti-epileptic medication. Despite years of treatment, Meera continued to have seizures, leading to repeated hospital visits. It wasn’t until six years later, when she underwent video-EEG monitoring, that her doctors realized she didn’t have epilepsy at all. Meera was finally diagnosed with dissociative seizures, a condition linked to unresolved emotional trauma. After starting psychotherapy, her seizures significantly reduced.
Meera’s case is not unique—many people, especially young women, are living with undiagnosed dissociative seizures. Getting the right diagnosis can make all the difference.
How Are Dissociative Seizures Different from Epileptic Seizures?
One of the reasons dissociative seizures are often mistaken for epilepsy is that they look so similar. But while they might appear the same on the surface, there are important differences that can help doctors tell them apart. Recognizing these differences is key to getting the right treatment.
Key Differences Between Dissociative and Epileptic Seizures
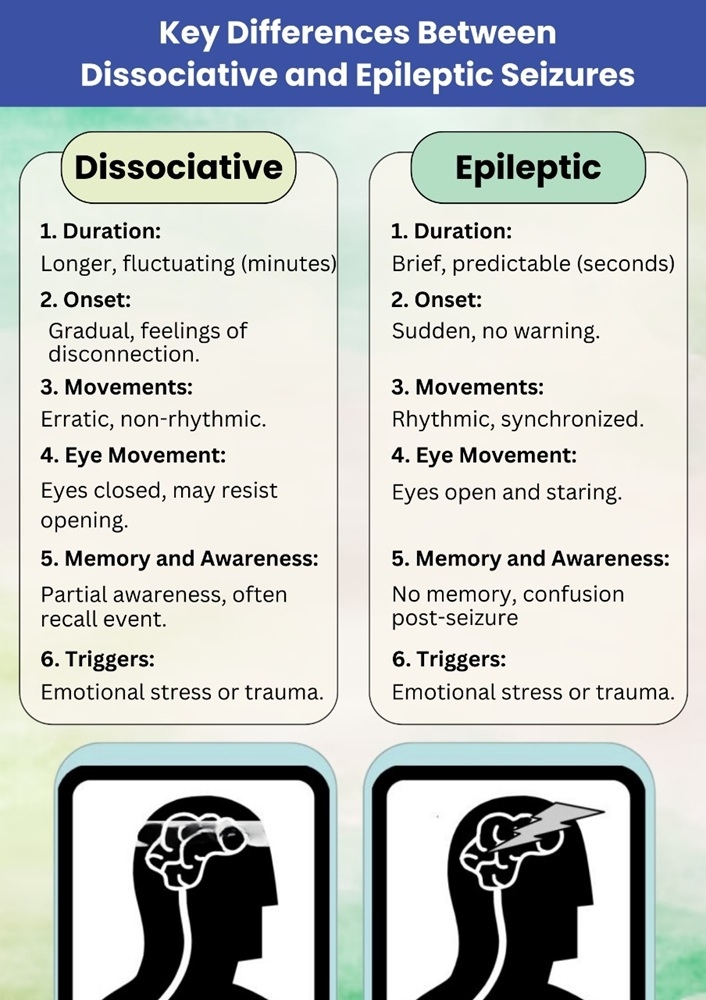
- Duration: Dissociative seizures tend to last longer than epileptic seizures. While epileptic seizures are typically brief and follow a predictable pattern, dissociative seizures may go on for several minutes and have a more fluctuating course.
- Onset: Dissociative seizures often start gradually, with the person feeling disconnected or distant from their surroundings. Epileptic seizures, on the other hand, typically come on suddenly without warning.
- Movements: The movements in dissociative seizures can be more erratic and non-rhythmic. In contrast, epileptic seizures usually involve rhythmic and synchronized movements. Side-to-side head movements, exaggerated body movements, or thrashing are more common in dissociative seizures.
- Eye Movement: In epileptic seizures, patients often have open, staring eyes. In dissociative seizures, the eyes are usually tightly closed, and the person may resist attempts to open them.
- Memory and Awareness: After an epileptic seizure, patients often have no memory of the event and may be confused. However, people with dissociative seizures may remain partially aware of their surroundings and often remember what happened during the episode.
- Triggers: Dissociative seizures are more likely to be triggered by emotional stress, trauma, or psychological factors, while epileptic seizures are caused by abnormal brain activity and may be triggered by things like lack of sleep or flashing lights.
Using Video-EEG Monitoring for Diagnosis
One of the most effective tools for distinguishing between dissociative seizures and epilepsy is video-EEG monitoring. This method records both the physical movements and brain activity during a seizure. In dissociative seizures, the EEG shows normal brain activity, confirming that the seizures are not epileptic. This helps doctors make an accurate diagnosis and avoid unnecessary epilepsy treatments.
The Impact of Misdiagnosis: A Case of Unnecessary Treatment
Unfortunately, many people with dissociative seizures are mistakenly diagnosed with epilepsy and prescribed anti-epileptic drugs, which are not only ineffective but can also cause harm. In some cases, patients experience significant side effects from these medications without any improvement in their seizures.
Rahul, a 28-year-old man from Mumbai, was diagnosed with epilepsy at 22 after experiencing frequent seizures. Despite taking multiple anti-epileptic medications, his seizures continued. After several years of ineffective treatment, Rahul was finally diagnosed with dissociative seizures through video-EEG monitoring. He was able to stop his epilepsy medications and begin psychotherapy, which helped reduce his seizures. However, the years of unnecessary medication had already caused liver damage, which highlights the risks of misdiagnosis.
The Role of Comorbid Anxiety and Depression
Many people with dissociative seizures also struggle with anxiety and depression. These conditions often go hand in hand with dissociative seizures and can worsen the severity and frequency of the episodes. For example, someone dealing with untreated anxiety or depression may find that their emotional distress triggers more frequent seizures.
Why Are Anxiety and Depression Common in Dissociative Seizures?
Dissociative seizures are often linked to emotional trauma or psychological stress. Many patients have experienced difficult life events, such as childhood abuse, family conflict, or overwhelming stress, which can lead to feelings of anxiety and depression. The emotional burden can become overwhelming, and dissociative seizures may develop as a coping mechanism for these unresolved feelings.
Managing Anxiety and Depression in Dissociative Seizures
To effectively treat dissociative seizures, it's important to address any underlying mental health conditions. Here are some key steps in managing anxiety and depression:
- Psychotherapy: Cognitive-behavioral therapy (CBT) is one of the most effective treatments for managing both dissociative seizures and comorbid anxiety or depression. CBT helps patients recognize negative thought patterns and develop healthier ways to cope with stress and emotional triggers.
- Medication: In some cases, antidepressants or anti-anxiety medications may be prescribed to help manage anxiety and depression. These medications can help stabilize mood and reduce the emotional distress that often triggers dissociative seizures.
- Stress-Management Techniques: Learning relaxation techniques such as deep breathing, mindfulness, or meditation can help patients manage their stress levels and reduce the likelihood of seizures.
- Support Groups: Joining a support group can provide emotional support and a sense of community for people with dissociative seizures, helping them feel less isolated in their struggle.
Breaking the Stigma: Understanding the Mind-Body Connection
One of the biggest barriers to diagnosing and treating dissociative seizures is the stigma around mental health. In India, where mental health conditions are often misunderstood or ignored, many people are reluctant to accept that their seizures could be caused by emotional or psychological factors.
It’s important to understand that dissociative seizures are just as real and debilitating as epileptic seizures. They are not “faked” or “all in your head.” Dissociative seizures are a legitimate medical condition that results from the mind and body’s complex response to stress or trauma.
By raising awareness and reducing the stigma around mental health, we can ensure that people with dissociative seizures receive the right diagnosis and treatment sooner, helping them lead healthier, more fulfilling lives.
Conclusion: Hope for Healing
Dissociative seizures are a complex condition, often misunderstood and misdiagnosed as epilepsy. But with proper diagnosis, treatment, and understanding of the mind-body connection, people with dissociative seizures can find relief and healing. Early diagnosis through tools like video-EEG monitoring can prevent years of unnecessary medication and suffering, allowing patients to focus on the psychological causes of their seizures.
If you or a loved one has been struggling with seizures that don’t respond to treatment, it’s important to consider the possibility of dissociative seizures. Seeking help from a mental health professional and exploring psychotherapy can make a significant difference.
Remember, healing is possible, and understanding the emotional triggers behind dissociative seizures can lead to lasting recovery.
TAGS: What Are Dissociative Seizures?, Difference between a psychogenic seizure and an epileptic seizure?, Can dissociative seizures be cured?, Dissociative seizures treatment, Dissociative seizures causes, How to deal with epilepsy depression?, How to overcome seizure anxiety?, Can seizures cause anxiety and depression?
Disclaimer:
All characters and events depicted in this blog are entirely fictional. Any resemblance to actual persons, living or dead, is purely coincidental. The content is intended for informational purposes only and should not be considered as medical advice. Always consult a qualified healthcare professional for medical concerns.




No comments yet. Be the first to comment!