Obsessive-Compulsive Disorder (OCD) is a mental health condition that's often not fully understood or taken seriously in our daily conversations or through the media. However, it's crucial to realize that OCD is a significant mental health issue that can severely impact individuals who experience it. This article aims to shed light on what OCD entails, its symptoms, and the ways in which it can affect people, with a specific focus on how it is perceived and managed in the Indian context.
OCD is more than just a passing quirk or preference for neatness. It is a complex mental health disorder that can profoundly disrupt a person's daily life, causing distress and impairing their ability to function. Those living with OCD may experience intrusive, persistent thoughts (obsessions) that lead to repetitive behaviors or mental acts (compulsions) in an attempt to alleviate the anxiety brought on by these thoughts.
Understanding and acknowledging OCD as a legitimate condition is key to providing support and effective treatment. By fostering empathy and dispelling misconceptions surrounding OCD, we can create a more inclusive and compassionate environment for individuals grappling with this disorder. It is essential to seek professional help and explore various treatment options to manage OCD effectively.
In recent years, emerging therapies like Repetitive Transcranial Magnetic Stimulation (rTMS) have shown promise in treating OCD by targeting specific areas of the brain associated with the disorder. This innovative approach offers hope for individuals who have not found relief through traditional treatments.
Understanding Obsessive-Compulsive Disorder (OCD)
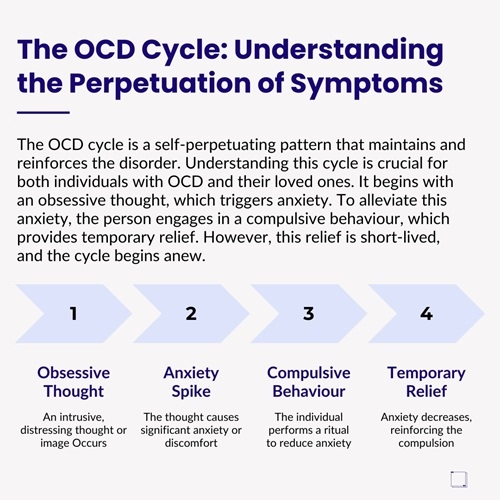
Obsessive-Compulsive Disorder, commonly known as OCD, is a mental health condition where a person experiences obsessions, compulsions, or a mix of both. Obsessions are those intrusive and undesirable thoughts, images, or urges that really bother a person. Picture this - someone might constantly worry about germs making them sick or feel a pressing need to double-check everything before leaving the house.
Now, compulsions are the actions or mental routines that a person feels they have to do to calm down the anxiety caused by these plaguing obsessions. Think of it like a pattern or ritual that a person follows to feel safe. For example, a person who is terrified of germs might wash their hands over and over again, like a never-ending cycle of scrubbing.
OCD can be tough because these thoughts and actions take up a lot of time and can interfere with someone's daily life. It's like having a bully in your head that makes you think and do things you don't even really want to. So, if you know someone battling OCD, they might need a bit of understanding and support to navigate through their world of intrusive thoughts and never-ending rituals.

About the Author
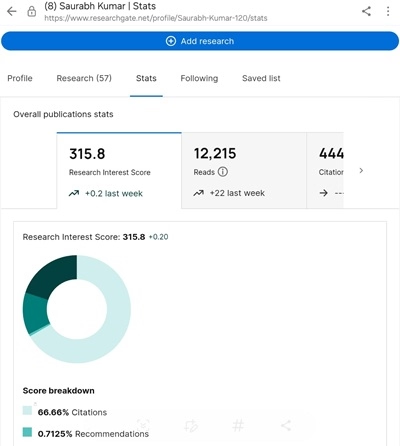
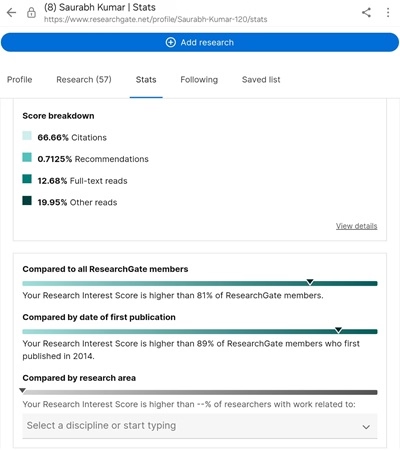
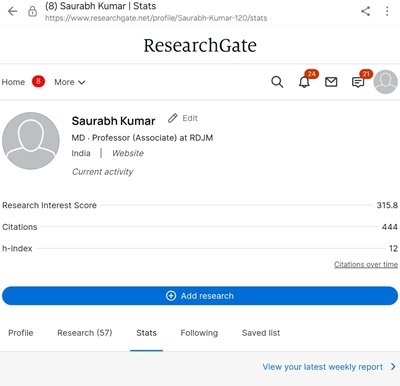
Dr. Saurabh Kumar
Dr. Saurabh Kumar is a distinguished expert in mental health, having authored numerous influential articles on ResearchGate. His research focuses on innovative approaches to mental health care and treatment. His work contributes significantly to advancing the understanding and improvement of mental health practices.
Prevalence and Cultural Context in India
Obsessive-Compulsive Disorder (OCD) is a widespread condition that affects around 2-3% of the global population. However, its impact in India is particularly worrying. OCD typically shows up during the teenage years or early adulthood and usually sticks around if not dealt with properly. In India, cultural beliefs and the negative view around mental health problems often result in people not reporting their symptoms and delays in getting a diagnosis. This lack of recognition and late diagnosis tends to make the condition worse.
One interesting thing to note is how cultural aspects in India heavily influence the types of obsessions and compulsions people experience with OCD. For instance, compared to other regions, religious worries are more common in India. These can take the form of fears related to disrespecting religious beliefs or not following religious traditions correctly. Religion holds a significant place in Indian society, so it's not surprising that these thoughts become a focal point for individuals struggling with OCD.
The specific cultural context in India not only influences how OCD shows itself but also impacts how others perceive it. Sometimes, because of this cultural lens, people may misinterpret symptoms or provide interventions that are not entirely appropriate for the individual's needs. The interplay between cultural beliefs and mental health challenges like OCD can make it tricky for individuals to seek help and receive the right treatment.
Understanding OCD Through Real-Life Examples
To better comprehend the complexities and effects of OCD, let's explore three relatable scenarios that showcase how this disorder can influence everyday routines and activities:
1. Rahul's Constant Cleaning: Meet Rahul, a 25-year-old software engineer residing in Bangalore. Rahul is fixated on the belief that his living space is contaminated. Even though he logically understands that his home is clean, he finds himself spending countless hours each day scrubbing every surface and compulsively washing his hands. This repetitive behavior has taken a toll on his skin, leading to severe damage, and has caused him to withdraw from social interactions. His entire life has become consumed by these cleaning rituals, making it challenging for him to concentrate on his career and nurture meaningful relationships.
2. Anita's Fear of Harming Others: Imagine Anita, a 30-year-old school teacher based in Delhi, who constantly battles intrusive thoughts about causing harm to her loved ones. While she is aware that she would never act on these distressing thoughts, the fear of losing control overwhelms her. To cope with this anxiety, Anita avoids sharp objects and seeks constant reassurance from her family members. These compulsive actions have a significant impact on her daily life, making it difficult for her to function normally and enjoy a fulfilling quality of life.
3. Aarav's Religious Worries: Let's consider Aarav, a 20-year-old college student from Varanasi, who grapples with intrusive thoughts that he has committed blasphemy. This leads him to engage in hours of prayer and perform various rituals to alleviate these distressing thoughts. Unfortunately, this obsessive behavior hampers his academic performance and social interactions, as his mind is preoccupied with the fear of offending his faith or divine entities.
These case studies shed light on the profound effects that OCD can have on an individual's daily activities and overall well-being. It showcases how this disorder can significantly impact personal, social, and professional aspects of one's life, highlighting the importance of recognizing and addressing OCD symptoms to ensure a better quality of life.
The Impact of Obsessive-Compulsive Disorder (OCD) on Daily Life
Obsessive-Compulsive Disorder (OCD) can have a profound impact on different aspects of our lives, from personal relationships to our performance at work or in school. In India, there is a prevalent stigma surrounding mental health issues, which can make these challenges feel even more overwhelming. People with OCD often find themselves facing discrimination and a lack of understanding, with their behaviors sometimes being misinterpreted as mere quirks or seen as spiritual disturbances.
This societal stigma not only adds more hurdles to seeking help but can also lead to delays in receiving proper treatment, ultimately exacerbating the outcomes of the disorder. To illustrate, consider Anita's situation, where her intrusive thoughts might be misconstrued as signs of spiritual possession rather than being recognized as symptoms of OCD. This misunderstanding could prompt her family to turn to religious healers for intervention instead of seeking the expertise of mental health professionals.
Similarly, let's examine Aarav's experience, where he might be unfairly judged for his rituals and obsessions, being branded as someone who lacks faith rather than being seen as someone grappling with a genuine psychiatric disorder. This misinterpretation not only hinders Aarav's journey towards recovery but also perpetuates the misconception that OCD is merely a matter of personal beliefs rather than a clinical condition that requires proper treatment and support.
The Biological and Psychological Basis of OCD
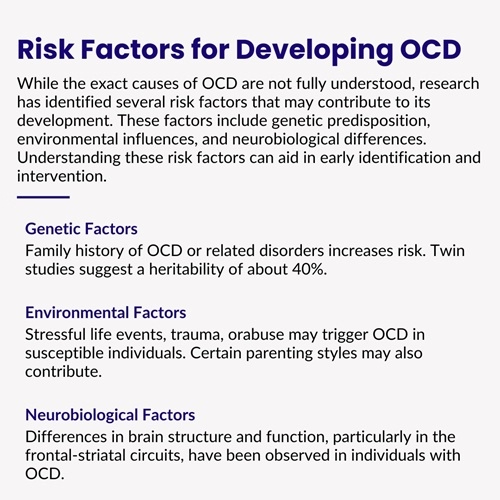
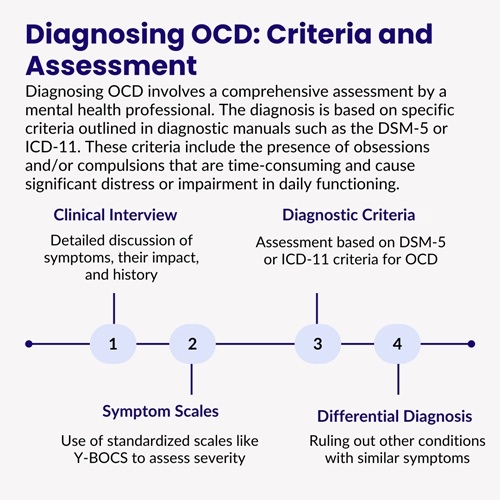
Obsessive-Compulsive Disorder (OCD) is a mental health condition that causes a person to have recurring thoughts and behaviors that are difficult to control. While the exact reasons why OCD develops are not completely understood, scientists think that it is a combination of genetic, brain-related, and environmental factors.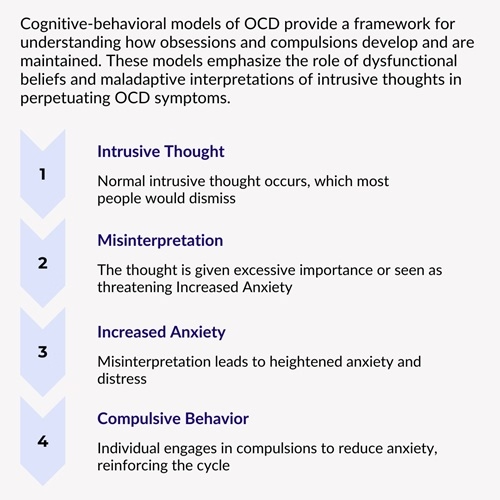
Studies have shown that there are certain abnormalities in the brain that may contribute to the development of OCD. Specifically, the orbitofrontal cortex, anterior cingulate cortex, and caudate nucleus - all areas of the brain - are suspected to play a role in the disorder. These parts of the brain are believed to be involved in functions such as recognizing errors, making decisions, and regulating emotions, all of which can go awry in people with OCD.
Furthermore, research has shown that neurotransmitters, which are chemicals that help transmit signals in the brain, such as serotonin and glutamate, may also be involved in OCD. Serotonin, in particular, seems to be a key player in the development of OCD, as many individuals with the disorder respond positively to medications that increase serotonin levels in the brain.
By gaining a better understanding of the biological and psychological factors that contribute to OCD, researchers hope to develop more effective treatments for individuals living with this challenging condition.

Prioritize your mental wellness— schedule a visit with the top psychiatric doctors in Patna now.
Comprehensive Treatment Approaches for OCD
Effective OCD treatment usually includes a mix of therapy and medication. One common treatment is cognitive-behavioral therapy (CBT), which helps change the way you think and behave. A specific type of CBT called Exposure and Response Prevention (ERP) is often used for OCD. This involves facing your fears gradually, without giving in to compulsions. In addition to therapy, doctors may also prescribe medications like Selective Serotonin Reuptake Inhibitors (SSRIs) to help manage symptoms. By combining therapy and medication, individuals with OCD can find relief and learn to better manage their condition.
Cognitive-Behavioral Therapy (CBT):
Cognitive-Behavioral Therapy (CBT) is a kind of therapy that's been found to work really well for treating Obsessive-Compulsive Disorder (OCD). One type of CBT, called Exposure and Response Prevention (ERP), is considered the best way to help people with OCD. How it works is that it helps individuals to face their fears without giving in to rituals or compulsions. For instance, someone who's terrified of germs might be asked to touch something they believe is dirty and then not wash their hands right after. This exposure technique helps to lower anxiety and stop the cycle of compulsive behaviors.
Studies have shown that ERP is highly effective in reducing symptoms for about 60 to 85 percent of patients. And the good news is that the positive effects can last for years even after the treatment is over.
Pharmacotherapy:
Pharmacotherapy involves using medications, like SSRIs such as fluoxetine, sertraline, and fluvoxamine, along with Cognitive Behavioral Therapy (CBT) to help with obsessive thoughts. These drugs can ease anxiety and distress caused by obsessions, which makes it easier for people to participate in Exposure and Response Prevention (ERP) therapy. Research has found that around 40-60% of patients feel some relief from symptoms when taking SSRIs. However, it's uncommon for medication alone to completely eliminate symptoms. Combining medication with CBT tends to be more successful in managing these challenges.
Repetitive Transcranial Magnetic Stimulation (rTMS):
Repetitive Transcranial Magnetic Stimulation (rTMS) is a new and innovative treatment for Obsessive-Compulsive Disorder (OCD). It's a procedure that doesn't involve any surgery or invasive techniques, so there's no need to worry about that. Basically, rTMS uses magnetic fields to target specific areas of the brain that are thought to be involved in OCD. These areas include the orbitofrontal cortex and the supplementary motor area, which are known to be hyperactive in people with OCD.
Research has shown that rTMS can be helpful in calming down these overactive brain circuits, and in turn, reduce OCD symptoms. Especially for patients who haven't gotten better with the usual treatments like therapy or medication, rTMS can offer a new hope. While it's not yet the go-to treatment for OCD, it definitely shows potential, especially for those tough cases that don't respond to other methods.
So, in simpler terms, rTMS is a cool way to use magnets to target specific parts of the brain that are causing OCD symptoms. By doing this, it might be able to help people feel better and manage their OCD more effectively. It's still being explored and researched, but it's exciting to think about the possibilities it holds for those who haven't found relief through traditional treatments.
Other Emerging Therapies:
Apart from using rTMS, researchers are also studying other treatments like deep brain stimulation (DBS) to help people with severe OCD. DBS involves putting small electrodes into certain areas of the brain to control how they work. This method, although more intrusive, has shown promise for people with OCD that hasn't responded well to other treatments. However, these approaches are still being tested and are generally only tried when other therapies haven't worked. Scientists are continuously looking for new ways to help people struggling with OCD, and these emerging treatments offer hope to those who haven't found relief through traditional methods.
Moving Towards a Better Understanding and Support for Obsessive-Compulsive Disorder
Obsessive-Compulsive Disorder (OCD) is a complex and challenging mental health issue that affects many people in India. It's important for us to learn more about the signs, reasons behind it, and the different ways to help those who have it. By doing so, we can offer better support to individuals dealing with this condition. It is crucial to know that OCD is a medical problem that can be treated effectively. It is not a flaw in someone's personality or a lack of spiritual strength.
With more knowledge, empathy, and access to proper care, people with OCD can live full, satisfying lives. As India grows in its understanding of mental health, it is crucial to create an environment where everyone feels comfortable asking for help with their mental health. Educating others and reducing the negative beliefs about mental health problems is key to ensure that those with OCD and other similar issues get the help and support they need to thrive in society.
Read More Research Case Report PDF
- Low-frequency Repetitive Transcranial Magnetic Stimulation for Treatment of Tourette Syndrome: A Naturalistic Study with 3 Months of Follow-up
- Effectiveness and Predictors of Response to 1-Hz Repetitive Transcranial Magnetic Stimulation in Patients With Obsessive-Compulsive Disorder
- Repetitive Transcranial magnetic stimulation (rTMS) over the supplementary motor area in the treatment of late onset OCD with Tourette's syndrome (TS)


As a psychologist, I often come across individuals and families who have mistaken OCD for being perfectionist or just a personality type. Just because of this misperception, the individual and family both suffer for years and years. Awareness regarding OCD and reaching out to a mental health practitioner are 2 steps to recovery.