In today's fast-paced world, stress has become a familiar companion. Whether it’s juggling work deadlines, family responsibilities, or financial concerns, everyone experiences stress at some point in their lives. However, the way we respond to stress can vary significantly from person to person. This blog explores the concept of stress, the importance of resilience in managing stress, and the impact both have on overall health. By understanding these concepts, we can learn to navigate life's challenges more effectively.
Understanding Stress: Not All Stress is Bad
Stress is a natural part of life. It is our body's response to any demand or threat, real or perceived. Stress can be both positive and negative:
- Eustress: This is the "good" stress that motivates us to perform better, such as the adrenaline rush before a big presentation or competition.
- Distress: This is the "bad" stress that can lead to anxiety, depression, and other health issues when experienced over long periods.
The concept of stress in psychiatry has evolved significantly over the years. Pioneered by Hans Selye in 1936 with the General Adaptation Syndrome (GAS), stress was initially described as a non-specific response of the body to any demand for change. Selye's work laid the foundation for modern stress research, differentiating between eustress and distress and recognizing stress as a significant factor in mental health and illness.
The Biological Underpinnings of Stress
When we experience stress, our bodies activate the Hypothalamic-Pituitary-Adrenal (HPA) Axis. This involves a cascade of hormonal responses starting from the hypothalamus, which releases Corticotropin-Releasing Hormone (CRH). CRH then stimulates the pituitary gland to produce Adrenocorticotropic Hormone (ACTH), which in turn signals the adrenal glands to release cortisol, the primary stress hormone.
Impact of Cortisol:
- Alters neurotransmitter balance in the brain, affecting mood and emotional regulation.
- Regulates metabolism and energy usage
- Modulates immune system function.
While cortisol is vital for survival, chronic stress can lead to prolonged cortisol secretion, resulting in negative effects on both mental and physical health. For instance, prolonged cortisol elevation can cause hippocampal atrophy (impacting memory and emotional regulation), amygdala hypertrophy (increasing anxiety and fear responses), and prefrontal cortex changes (impairing decision-making and executive functions).
The Interplay Between Stress and Psychiatric Disorders
Stress is a key factor in the development and maintenance of various psychiatric disorders. Let's explore how stress contributes to some common mental health conditions:
Depression: Chronic stress can lead to persistent activation of the HPA axis, resulting in elevated cortisol levels, neurotransmitter imbalances (such as serotonin and dopamine), and inflammation—all of which are associated with Major Depressive Disorder (MDD). For example, a 35-year-old software engineer from Bengaluru, constantly under high-pressure work conditions, began experiencing symptoms of depression, including fatigue, sleep disturbances, and persistent low mood. Over time, these symptoms worsened, and he was diagnosed with MDD.
Anxiety Disorders: Stress affects brain regions involved in anxiety regulation, such as the amygdala and prefrontal cortex. Chronic stress can enhance amygdala reactivity, increasing fear and anxiety responses. For instance, a young woman from Mumbai experienced chronic anxiety after a traumatic road accident. Despite the passage of time, her heightened anxiety persisted due to stress-induced changes in her brain circuits.
Post-Traumatic Stress Disorder (PTSD): Traumatic stress can lead to long-lasting changes in brain function and structure. PTSD is associated with amygdala hyperactivity, reduced hippocampal volume, and prefrontal cortex dysfunction. For example, a 40-year-old man from Delhi, who experienced childhood abuse, presented with symptoms of PTSD, including intrusive memories and emotional numbing.
Schizophrenia: The stress-diathesis model explains how stress interacts with genetic predisposition to trigger psychosis in vulnerable individuals. Early-life stress may alter brain development, increasing the risk of schizophrenia in genetically predisposed individuals.

Don’t Wait to Get the Support You Need – Call Us for an Appointment
Resilience: The Key to Coping with Stress
While stress is inevitable, our ability to cope with it—referred to as resilience—is a critical determinant of our mental health. Resilience is the capacity to adapt successfully and recover quickly from stressful or traumatic events. It is influenced by biological, psychological, and social factors.
Psychosocial Factors of Resilience:
Active Coping: The ability to utilize psychological and behavioral resources to cope with trauma or stressors.
Cognitive Flexibility: The capacity to dynamically adjust to external demands from trauma, based on acquired knowledge.
Social Support: Strong social relationships play a significant role in mitigating harm from trauma.
Neurobiological Factors of Resilience:
Glucocorticoids: Regulators of stress-related homeostasis.
HPA Axis: Governs the stress response and maintains resilience.
Neurotransmitters: Changes in dopamine, serotonin, and norepinephrine play a role in resilience.
Resilience in Action: Real-Life Scenarios
Case Example: Sunita, a 28-year-old nurse from Kolkata, faced immense stress during the COVID-19 pandemic. Her duties at the hospital, combined with concerns about her family's health, led to anxiety and emotional exhaustion. However, with strong social support from her colleagues and a practice of mindfulness, she developed resilience that helped her cope better. She focused on positive coping strategies, such as maintaining a work-life balance and engaging in recreational activities, which bolstered her mental health.
Building Resilience: Strategies and Interventions
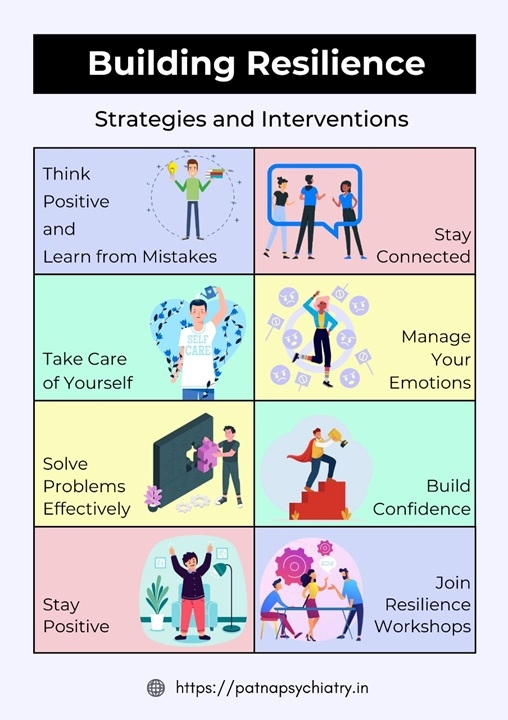
Resilience is not a static trait but a modifiable quality that can be enhanced through various interventions:
Mindfulness Training: Mindfulness-based practices have been effective in modifying stress recovery mechanisms.
Cognitive Training: Techniques like cognitive restructuring and problem-solving skills can enhance resilience.
Social Support Networks: Engaging in community support, family, and friends helps strengthen resilience.
Case Example: Rajesh, a 45-year-old school teacher in Chennai, developed resilience after experiencing significant life stressors, including the loss of a loved one and financial troubles. By seeking professional help and practicing mindfulness and cognitive-behavioral techniques, he built resilience and improved his emotional well-being.
Resilience and Physical Health
Resilience also plays a crucial role in physical health. Resilient individuals tend to have better outcomes in managing chronic conditions and recovering from surgeries. For example:
Chronic Pain Management: Patients with higher resilience levels suffer less distress and face chronic pain with optimism.
Surgery Recovery: Resilient patients undergoing major surgery experience less distress and recover more quickly.
Conclusion: Embracing Resilience for Better Health
Understanding the interplay between stress, resilience, and health is crucial for maintaining overall well-being. While stress is a part of life, developing resilience helps us navigate challenges more effectively. By adopting strategies like mindfulness, cognitive training, and strengthening social support, we can build resilience and improve both mental and physical health outcomes.
Incorporating resilience-building practices into daily life can help us not only survive but thrive amidst life's challenges. As the saying goes, "It’s not the load that breaks you down; it’s the way you carry it."
Explore More Topics:



It's important lesson to learn, how resilience can help to manage stress. Thank you sir for sharing this blog.
Very insightful thoughts..Psychiatric issues have a biological origin and is not a sign of any weakness. High time we realized this as a society.